The flu vaccine paradox: Are we making things worse?
03/24/2025 / By Willow Tohi

- Dr. Robert Malone highlights a counterintuitive finding that increased flu vaccination rates among the elderly correlate with higher influenza-related death rates, as shown in a 2005 study. He attributes this to the suppression of natural immunity and misclassification of flu-like illnesses caused by other pathogens.
- Malone warns that annual flu shots may cause “immune imprinting,” where the immune system becomes biased toward older virus strains, reducing its ability to respond effectively to new, evolving flu strains. This undermines the purpose of vaccination.
- He argues that partially effective flu vaccines can accelerate the evolution of vaccine-resistant viruses, making outbreaks harder to control. Malone asserts that imperfect vaccines cannot end influenza outbreaks and may worsen the situation.
- Malone challenges the narrative that the 1918 Spanish flu pandemic was primarily caused by the influenza virus, suggesting most deaths were due to secondary bacterial pneumonia. He advocates for prioritizing antibiotic research over mRNA flu vaccines.
- Unlike the U.S., most countries do not recommend universal flu vaccination. Malone argues that the U.S. approach is driven by the need to sustain vaccine manufacturing capacity rather than public health necessity, calling for transparency and informed consent in vaccination policies.
In a world where annual flu shots are marketed as a cornerstone of public health, Dr. Robert Malone, a renowned expert in vaccine development, has dropped a bombshell: much of what we’ve been told about influenza vaccination is, in his words, “propaganda.” In a recent essay titled “Deconstructing HHS: Influenza Vaccine Propaganda,” Malone challenges long-standing assumptions about flu vaccines, revealing startling data and historical context that demand a closer look.
The elderly paradox: More vaccines, more deaths?
One of the most shocking revelations in Malone’s essay is the claim that increasing annual influenza vaccination among the elderly is associated with higher influenza-related death rates. This counterintuitive finding is supported by a peer-reviewed study published in Archives of Internal Medicine in 2005. The study analyzed data from 1968 to 2001 and found that as flu vaccine coverage among the elderly rose from 15-20% to 65%, influenza-related mortality rates did not decline as expected.
“Natural immunity acquired by influenza infection works to prevent future ‘influenza-related’ deaths in the elderly,” Malone explains. “Vaccination to a specific influenza A virus strain (H1N1) does not improve natural immunity to that strain and, on average, increased influenza vaccine uptake increases all-cause ‘influenza-related’ death in the elderly.”
This raises serious questions about the efficacy of annual flu shots, particularly for older adults. Malone points out that “influenza-like illness” is often misattributed to the flu virus itself, when in fact, many other pathogens—such as respiratory syncytial virus (RSV), mycoplasma and coronaviruses—can cause similar symptoms. This misclassification inflates flu-related death statistics, much like the controversial “deaths with COVID” versus “deaths from COVID” debate.
Immune imprinting: Are flu shots backfiring?
Another critical issue Malone highlights is the phenomenon of “immune imprinting,” formerly known as “original antigenic sin.” This concept, first described in the 1960s, refers to how the immune system’s first exposure to a virus shapes its response to future infections.
“If you get ‘boosted’ every year with a suboptimal influenza vaccine, it sets your immune system up to be focused on last year’s virus rather than being better able to respond to tomorrow’s strain,” Malone writes. This immune bias can make individuals more susceptible to newly evolved flu strains, undermining the very purpose of vaccination.
This leads to a broader concern: the use of “leaky vaccines,” which are only partially effective at preventing infection and transmission. Malone warns that widespread deployment of such vaccines accelerates the evolution of vaccine-resistant viruses. “You cannot ‘vaccinate’ your way out of an outbreak of influenza with an imperfect vaccine,” he asserts. “If you try, you will only make matters worse.”
The 1918 Spanish flu: A misleading narrative?
Malone also takes aim at the historical narrative surrounding the 1918 Spanish flu pandemic, often cited as a justification for universal flu vaccination policies. He argues that most deaths during that pandemic were not caused by the influenza virus itself but by secondary bacterial pneumonia—a complication that could have been treated with antibiotics, had they been available at the time.
“If adequate doses of antibiotics had been available, the deaths would have been avoided,” Malone states. He suggests that instead of investing billions in new mRNA flu vaccines, the U.S. should prioritize domestic antibiotic research and manufacturing capacity.
A global perspective: Not everyone agrees
Malone notes that most countries do not recommend population-wide annual influenza vaccination. According to a 2016 global review of national immunization policies, only 59% of World Health Organization (WHO) member states have a national flu vaccine policy, and even then, programs typically target high-risk groups rather than the entire population.
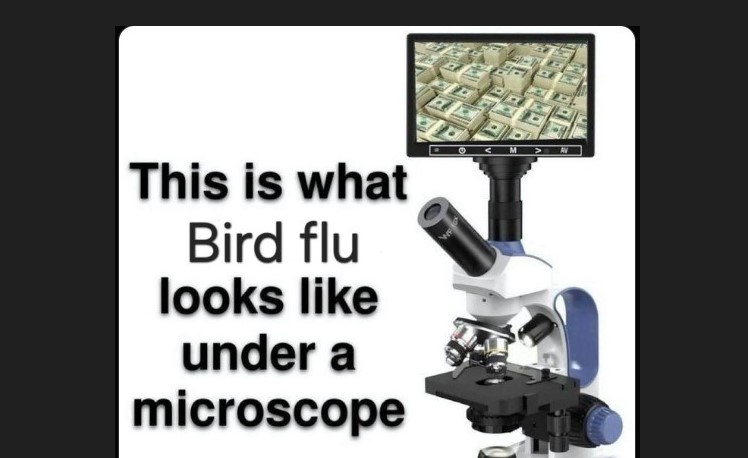
This stands in stark contrast to the U.S., where annual flu shots are heavily promoted for nearly everyone over six months old. Malone argues that this approach is driven less by public health necessity and more by the need to maintain influenza vaccine manufacturing capacity.
“You cannot build and mothball an influenza vaccine manufacturing facility for future use,” he explains. “You have to keep making influenza vaccines on a regular basis. And if you are going to make it, you need to have a market for the product.”
A call for transparency and informed consent
Malone’s essay is not an outright condemnation of vaccines but a plea for transparency, rigorous science and respect for individual autonomy. “I am an advocate for sound, well-justified medical practices,” he writes. “Vaccination is a medical procedure, and patients have the right to require informed consent.”
He calls for a shift in public health priorities, away from top-down mandates and toward personalized, physician-guided decision-making. “Making America Healthy Again will require respect for patients and their own personal bodily autonomy,” he concludes.
The bigger picture
Malone’s revelations come at a time when trust in public health institutions is at an all-time low. His essay challenges us to rethink long-held assumptions about flu vaccines and to demand better science, clearer communication and more ethical policies.
As Malone puts it, “Maybe MAHA [Make America Healthy Again] should think this through again?”
The question is: Will we?
Sources include:
Submit a correction >>
Tagged Under:
Censored Science, Dr. Robert Malone, Flu, health freedom, immune bias, immune system, influenza, medical violence, outbreak, real investigations, Vaccine deaths, vaccine injury, vaccine wars, vaccines
This article may contain statements that reflect the opinion of the author
RECENT NEWS & ARTICLES
FluShot.News is a fact-based public education website published by Flu Shot News Features, LLC.
All content copyright © 2018 by Flu Shot News Features, LLC.
Contact Us with Tips or Corrections
All trademarks, registered trademarks and servicemarks mentioned on this site are the property of their respective owners.